Posted on Friday, 25ᵗʰ September, 2020
The Lantern Alliance spoke to Kylie Wales, Honorary Senior Lecture and occupational therapist from the University of Newcastle about the importance of ‘personhood’ when approaching food and dining in aged care, and the difference between customer service and quality customer experience.

Service is the execution of a task for someone. Bringing a plate of food to the table and placing it in front of a diner is ‘service’. Experience is how the diner feels and responds to the service.
To further the example, if the food service staff are silent and avoid eye-contact, the chances are the diner won’t feel very good about the experience. However, if the diner is greeted by name, the meal is described to them, assistance is offered and the diner feels cared for, the experience is very different.
For mealtimes, the dining experience is equally if not more important than the service. Ideally the two work hand-in-hand so that residents can look forward to mealtimes as positive, relaxing experiences.
According to Kylie, mealtimes in aged care have also been used as a service-oriented activity, where many of the ‘services’ required by individuals can be administered while everyone is in one place.
For example, medication and in some cases, physical therapy have been part of the dining experience for aged care residents.
But as Kylie pointed out, mealtimes need to be reserved for the dining experience, and effort needs to be made to ensure residents are able to enjoy all aspects of the meal. This includes the social aspect, the food experience and a comfortable, welcoming environment which encourages joy and appreciation of food.
By placing personhood - an individual’s right to make their own decisions - at the centre of the dining experience, the enjoyment of mealtimes, and food are greatly enhanced.


Allowing residents to make their own choices is at the heart of the New aged care standards, and when it comes to food in aged care, the importance of informed choices cannot be overstated. There are many seemingly small changes which can easily be made to enhance your resident’s dining experience.
Allow residents to make choices about their food beyond the meal they would like to eat - for example simply placing condiments on each table so people are able to season their food exactly how they like it, rather than having to eat food not quite to their taste, or having to wait for someone to bring condiments to them.

As cognitive decline increases, the signals which trigger appetite often take longer to register so tuning into an individual’s needs on a daily basis is a large part of ‘person-centred’ dining.
What worked yesterday may not be appropriate today so checking in with how residents are feeling can assist staff and carers adjust the level of help to suit the exact needs of the individual. Assistance with eating is a common example where ability can vary depending on the type of food, and how well the resident is coping in the moment.
Kylie also recommends taking simple steps to help prepare people for a meal and stimulate appetite, which will help to enhance the overall dining experience.
For example, when escorting a resident from their room to the dining room, discuss the meal; talk about what the chef has prepared, what other foods the person likes - even what memories are associated with certain foods.
Offering a glass of water or juice prior to serving a meal can also help by moistening the mouth and preparing the digestive system.
Aroma is also an important part of dining and food. Essential dining areas don’t smell of cleaning products or air fresheners.
Delicious smells such as coffee brewing, bread or cakes baking, or the smell of roast chicken are instant appetite triggers and can help to create excitement about the meal. Aroma is also closely linked to memory and can help residents recall favourite meals and the events in their lives associated with those memories.

One of the simplest ways to make a dining area more welcoming and relaxing is to ensure the following:
1. Keep dining areas for eating and nothing else
Find a space outside of the dining area - and out of sight of the diners - for all equipment such as walkers and medication trolleys. These can detract from the enjoyment of food and socialisation; they create clutter and detract from the atmosphere.
2. Keep the dining experience and medication separate.
Medication and physical therapy have no place in a dining room. As Kylie emphasised, “If it would not happen in a restaurant or cafe, it should not happen in an aged care dining room.”
If it is essential for medication to be taken during a meal, it should be administered discreetly. It is preferable for medication to be taken prior to, or directly after the meal in the privacy of the residents’ room.
The combination of these small, simple changes go a long way in helping residents experience mealtimes in an enjoyable, social and calm atmosphere designed specifically for dining.

Disclaimer: The content of this article is created for inspiration purposes only. It is not intended as clinical, medical or nutritional advice.
Related Articles
Top recipes
-
Cream of Chicken Soup with Turmeric, Ginger and Shallots -
Hearty Chicken Soup -
Turmeric Coconut Chicken Curry -
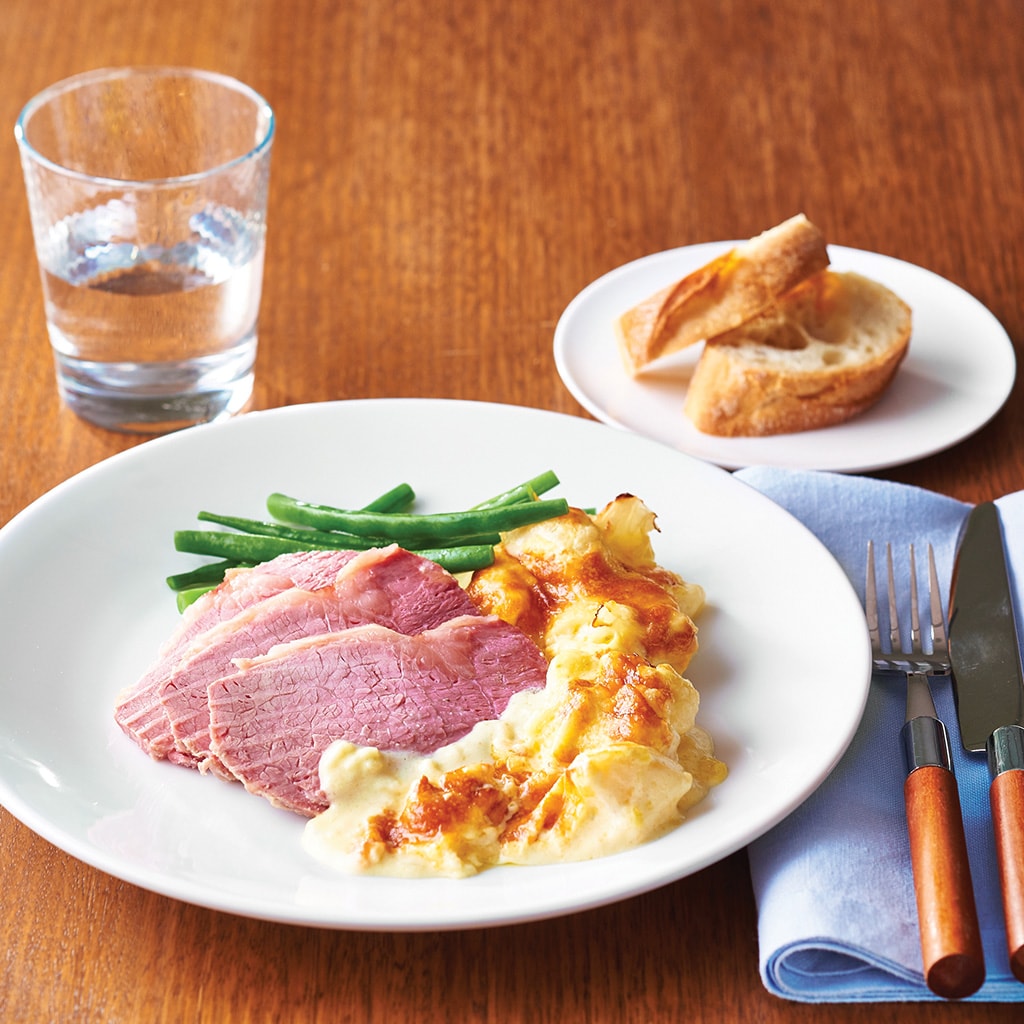
Potato and Cauliflower Cheese Mornay -
Citrus Poached Salmon Salad -
Grilled Chicken Breast, Cauliflower Puree -
Chicken Mornay Lasagne -
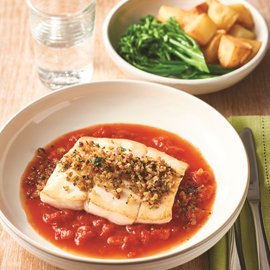
Provencal Fish Cacciatore -
Peri Peri Roast Chicken -
Chicken Ratatouille -
Chicken Parmigiana Pie -
Citrus Fresh Pannacotta -
Cheesecake Passion -
Lemon Meringue Pie
Related Products
Log in or Create an account to access:
- Get access to this content
- Discover the latest culinary trends
- Explore and save your favourite recipes
- Watch free video training courses for chefs