Updated on Thursday, 18ᵗʰ June, 2020

Wendy Foster
Speech Pathologist
Swallowing is a reflex as essential to life as breathing. While many of us barely notice how often we swallow each day, people who have trouble swallowing find it significantly impacts their lives. If you can’t swallow, simple things like eating, drinking and taking medicines become a serious challenge and can lead to dehydration, poor nutrition, and poor health.
To better understand the condition, we spoke to Wendy Forster, a certified practicing speech pathologist and Owner/Director at Adult Speech Pathology. Forster explained how it affects the elderly and what an aged care chef needs to know when preparing food and beverages for residents who may have swallowing difficulties.
Forster explained the condition, known as dysphagia, is a common symptom. Anyone, at any stage of life, can have trouble swallowing, although people over 65 years are more likely to experience it.
“In an aged care facility, dysphagia can affect between 55-68% of residents. One in three people with Parkinson’s disease and four out of every five people with dementia develop dysphagia,” Forster said.
“Dysphagia is common because it’s a symptom of many different underlying conditions; for example, a stroke, brain tumour, Motor Neuron Disease, Parkinson’s disease or dementia. The symptoms can develop gradually as a progressive disease advances, or suddenly, due to a stroke or brain injury.”
Forster assesses swallowing problems among aged care residents and recommends suitable approaches to ensure residents can still eat and drink well. She identifies a number of early warning signs to look out for:
- High plate waste, especially avoiding certain textures
- Coughing when eating or drinking or vomiting immediately after eating
- Slow eating, or moving food around in the mouth without swallowing
- Excess saliva, drooling, gurgling voice
- Unexplained weight loss
- Respiratory infections without known cause
- Slurred speech
When it comes to the type of food and drink someone with dysphagia needs, the texture modification depends on the severity of the swallowing difficulties.
A swallowing assessment will determine if food should be modified to a soft texture, minced and moist or smooth purée. “Food often contributes to a resident’s emotional nourishment and quality of life so we don’t want to over-modify food textures. Instead we aim for the highest level of texture that a person can safely manage and swallow. This means they can still enjoy the experience of food and get the nutrients they need,” Forster explained.
Forster recognises innovation in texture modification presentation is making a difference for residents with swallowing difficulties. “Thankfully, many foods are naturally soft. But we’re also seeing chefs develop inventive ways to prepare foods to be visually appealing, so residents with dysphagia don’t miss out.”
“In the warmer months, cold food such as soft sandwiches, pikelets, and potato salads, cold roast vegetable or pasta salad are delicious dysphagia-friendly options,” Forster suggested.
Fluids also need to be thickened to help the swallowing process. A nectar-form of juice is ideal, but other liquids can be thickened too. “The process of swallowing is triggered when food or liquid moves to a certain point at the back of the tongue. Slowing this process down with soft, slow moving food and liquid creates the right conditions to be swallowed easily,” Forster said.

Dysphagia Warning Signs Checklist
A helpful checklist to identify early dysphagia warning signs

Disclaimer: The content of this article is created for inspiration purposes only. It is not intended as clinical, medical or nutritional advice.
Top recipes
-
-
Fish Pie with Potato Top -
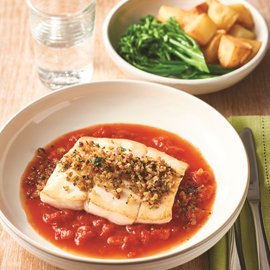
Provencal Fish Cacciatore -
Roast Salmon with Corn Puree -
Chicken Ratatouille -
Chicken Mornay Lasagne -
Creamy Tuna and Tomato Vol au Vents -
Slow Cooked Lamb Shoulder -
Lentil and Cauliflower Dhal -
Chicken Parmigiana Pie -
Diced Steak and Mushroom Goulash -
Poached Chicken with Peas, Zucchini and Leek -
Broccoli and Cheddar Soup -
Asian style beef broth
Related Products
Log in or Create an account to access:
- Get access to this content
- Discover the latest culinary trends
- Explore and save your favourite recipes
- Watch free video training courses for chefs